I am addressing preventing MRSA infection today by special request. It is a common condition that I often encountered when providing primary health care. Chances are, you may have experienced it or know someone who has. Or, you’ve watched Dr. Pimple Popper.
What is MRSA?
Well, it is a type of staphylococcus aureus- called “staph” for short- that is resistant to certain antibiotics. It gets its name from resistance to methicillin, a penicillin-type of antibiotic. MRSA stands for “methicillin resistant staphylococcus aureus”. MRSA is so much easier and quicker to say.
So what is staph?
Staph is a bacteria that lives on the skin or in soft tissue, like muscle or connective tissue. Most of us have staph living on our skin, but it really likes hanging out in your groin, buttocks, armpits and up in your nose. Now, just hanging out, it causes no problems. This is called colonization. Infection occurs when it gets inside the skin or into the soft tissue structures like connective tissue and muscle. Then, it causes symptoms. Staph can cause infections like pneumonia, endocarditis (infection in the heart), joint infections, and sepsis, a serious infection in the bloodstream. To recap: staph can live on your skin but if it gets into the skin or into a surgical site can cause an infection.
How bad does a staph infection get?
Superficial infections are generally mild. Follicles commonly get infected and this can cause a small abscess or furuncle. Collections of abscesses are called caruncles. These abscesses can be painful. Surgical sites can become infected; these are more serious than superficial skin infections. Pneumonia can require hospitalization. Sepsis is a severe infection in the bloodstream that requires hospitalization and immediate treatment. It is characterized by fever and chills and can cause organ system damage.
Where do we get staph from?
Initially, MRSA was associated with hospital stays. Think about it: who is in a hospital? Sick people getting antibiotics who are in a compromised immune state. Staph can live on surfaces for hours to weeks. This includes:
- Bed linens and towels
- Athletic equipment
- Medical equipment
- High touch surfaces such as remotes and light switches
- Utensils
- Clothes
Sick people in a hospital can be exposed and get staph there. There are other resistant bacterial infections that are associated with hospital stays including VRE (vancomycin-resistant enterococcus) but these do not occur in the community. MRSA “escaped” the hospital and is now readily transmitted in community settings. like barracks, dormitories, and sports teams that share equipment or have skin-to-skin contact (think football and wrestling). We now call these MRSA strains “hospital-acquired MRSA” (HA-MRSA) and “community-acquired MRSA” (CA-MRSA).
Who gets MRSA?
Anyone can get it. About 30% of us are colonized with staph at any time; some of that will be MRSA. Some folks are higher risk that others. Drug injectors are 16 times more likely to get MRSA than the general public. Also at increased risk of getting CA-MRSA infections are:
- Military
- Students, particularly living in dorms
- Health care providers
- Farmers, livestock workers, veterinarians
- Inmates
- Athletes
- Pets – yes, sometimes your pet can have MRSA too!
What are the symptoms or a MRSA infection?
Patients often told me they had a “spider bite”. Did they SEE the spider? Nope. OK then, it is most likely a MRSA infection. Patients often present with a red, painful swollen area on their skin (OK, it kinda looks like a spider bite). It might look like a pimple and is often larger than that by the time patients come in to clinic. If it is taut and feels fluctuant, then it can be drained and material sent for culture.
I have seen MRSA infections of a joint – the affected joint can be very swollen, hot and red. There is loss of range of motion caused by the swelling. Surgical sites can be very red and swollen and tender. (Public service announcement: please mind your post-surgical instructions to a T! This is what we want to prevent, so DO AS YOU ARE TOLD!)
How is MRSA diagnosed?
Ideally, MRSA is diagnosed by a culture taken from the affected area. A culture and sensitivity, as it is called, can take 48 hours to be processed. It will show which bacteria grew out and which antibiotics will work. That is what tells us if it is MRSA or some other bacteria. Sometimes the area is too small to attempt to drain, so antibiotics can be used empirically. That means we make an educated guess (doctors hate it when I say that) and provide an antibiotic based upon what we THINK we are treating.
How is MRSA treated?
Well that has changed some. We are trying to become better stewards of antibiotic use in medicine, so the trend is currently to incise and drain an abscess. That usually does it by decreasing the bacterial load so your immune system can fix the rest of the infection. Sometimes hot packs are used to bring blood flow to the area and bring an abscess “to a head”, triggering natural drainage.
If there is an accompanying cellulitis (swollen hot red skin, no pus) then an antibiotic may be given. Antibiotics are also used in patients who have recurrence after incision and drainage, those who have multiple comorbidities like diabetes, have immune compromise, or have abscesses that are not easily drained, like those on the face or hands. Deep skin structure infections like a joint infection may require surgery to remove diseased tissue. Some patients require hospitalization, including those with osteomyelitis (bone infection), endocarditis (heart infection) and pneumonia or sepsis. Sepsis requires immediate treatment and is considered life-threatening.
Are there any other treatments for MRSA?
Personal and environmental hygiene are very important in preventing recurrences and transmission to close contacts.
- Keep wounds clean and bandaged.
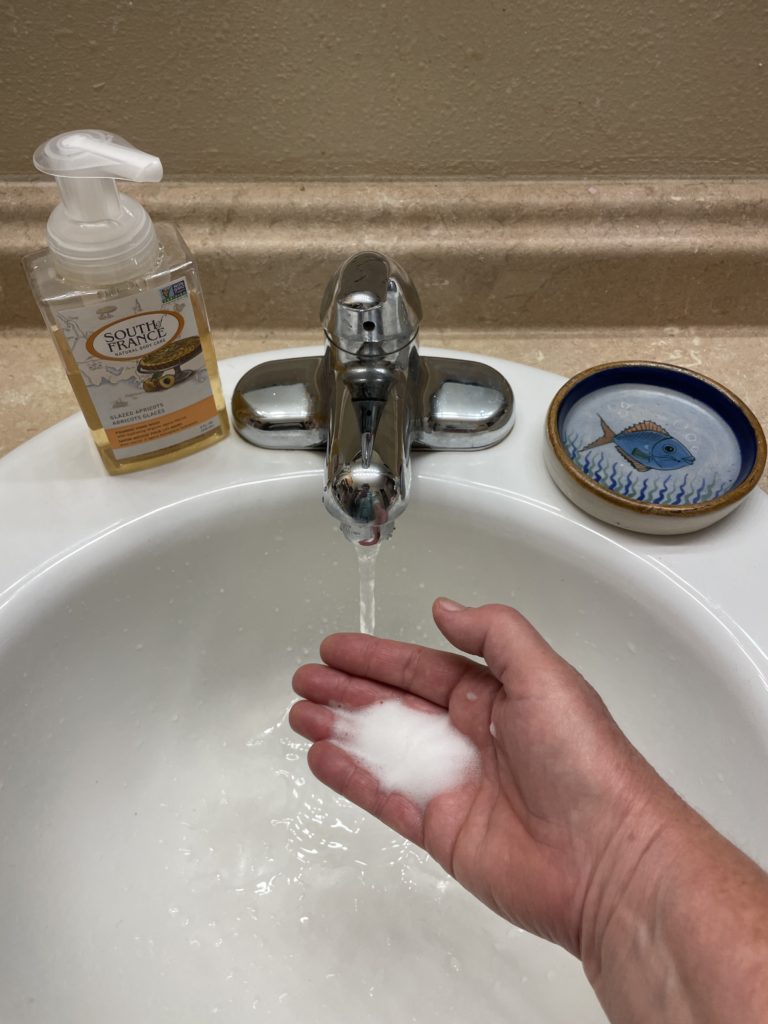
- Hand washing, hand washing hand washing. Did I say hand washing? Soap and water are best, but hand sanitizer works, too. This decreases bacterial load on the hands and can prevent contamination of subsequently touched surfaces.
- Use antiseptic cleaner or wipes to clean high touch surfaces such as light switches, toilet seats, door knobs, remotes and countertops..
- Don’t share or reuse objects like razors, towels and washcloths, and linens.
- Laundry can be washed in hot or cold water, but be sure and dry in a dryer.
- When working out, clean surfaces before touching, such as the bench or mat you are going to use.
What about decolonization?
Decolonization means attempting to decrease the number of colonized bacteria in the nose to prevent recurrence or transmission to close contacts. This is sometimes done when multiple cases are associated with a person carrying MRSA, or they are having frequent recurrence of infections. A topical antibiotic ointment is applied to the nostrils. Sometimes, a skin rinse is used called chlorhexidine.
Anything else?
Yes, please know these infections are common, and that they are usually mild and easily treated. Like c diff, these infections are another reason why we health care providers are supposed to be good stewards of antibiotic use.
Please join me next time for a discussion about post-infectious IBS, a common occurrence after having c diff.
MRSA (Staph Infection: What It Is, Symptoms & Treatment (clevelandclinic.org)
MRSA: Treatment, causes, and symptoms (medicalnewstoday.com)