For many years I had discussions with my patients about how we as health care providers needed to be good stewards of antibiotic use. It usually came in the context of explaining to a patient why I thought they didn’t need an antibiotic for their condition. Little did I know that that I would develop an antibiotic-related infection and become a poster child for antibiotic stewardship myself.
What is antibiotic stewardship?
Stewardship means “taking care of something or supervising a process”. When applied to the use of antibiotics, stewardship simply means to pay attention to how they are being prescribed. It is important to prescribe the RIGHT antibiotic for the RIGHT condition, at the RIGHT dose for the RIGHT duration of time. Health care providers rely on clinical studies and evidence-based guidelines when selecting an antibiotic for a given condition.
Antibiotic stewardship is defined by the CDC as the effort to measure antibiotic prescribing; to improve antibiotic prescribing by clinicians and use by patients so that antibiotics are only prescribed and used when needed; to minimize misdiagnoses or delayed diagnoses leading to underuse of antibiotics; and to ensure that the right drug, dose, and duration are selected when an antibiotic is needed.
Why does stewardship matter?
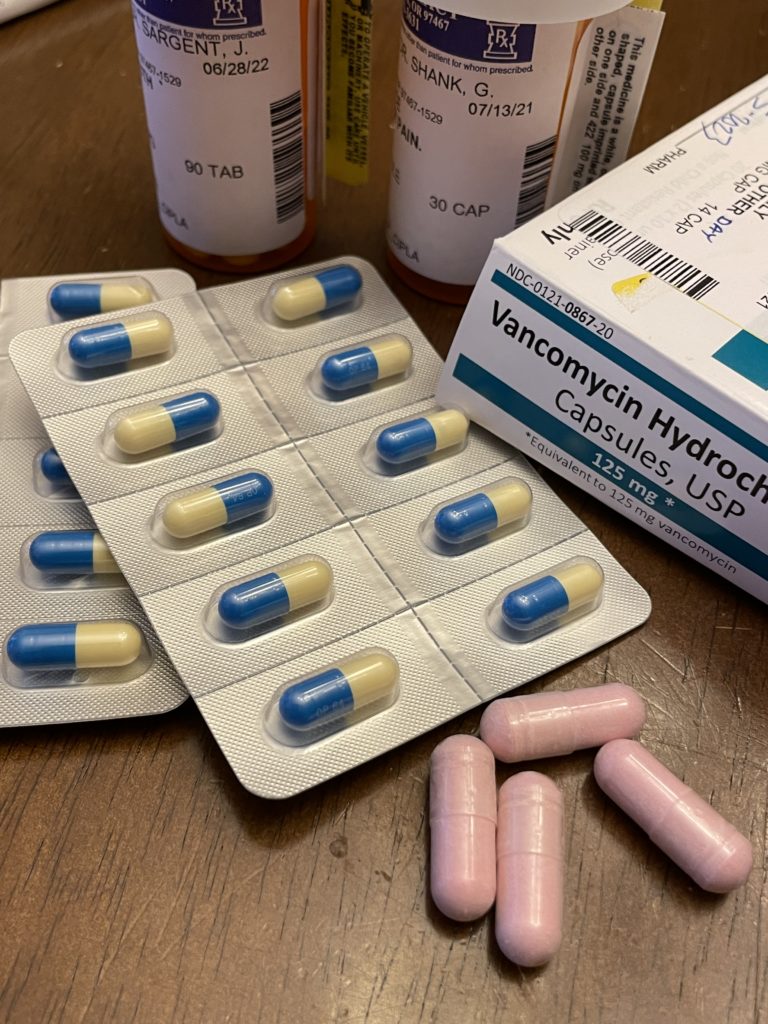
Antibiotic resistance is becoming a huge problem. Bacteria that cause serious infections are able to develop resistance when antibiotics are used inappropriately. There are now drug-resistance bacterial strains, such as vancomycin-resistant enterococci and extended beta lactamase resistant strains, that can really wreak havoc, causing significant disability or death.
So why don’t we just give different antibiotics?
A given antibiotic kills a range of certain bacteria. In other words, antibiotics aren’t “one size fits all”. Antibiotics penetrate different tissues differently. Some work better in one organ than another. Some antibiotics (broad-spectrum) kill a wider range of bacteria. They all kill off a range of friendly bacteria, too. That leads to side effects like diarrhea and secondary infections such as c diff. While we can give a different antibiotic in some cases, that often means hospitalization for intravenous antibiotics. Unfortunately, there aren’t enough NEW antibiotics being developed.
Why aren’t there more antibiotics in the pipeline?
Bringing a new antibiotic to the market is time-consuming. It can take 10-15 years to go from bench trials to phase three clinical trials. Then the drug is “brought to market” meaning the company must plan for manufacturing and marketing it. The cost of this process ranges from 1-3 billion dollars, and these costs are often not recouped. Many start-up pharmaceutical companies fail after developing a promising drug, going bankrupt before they can get their new antibiotic to market. Investors are more likely to support drugs taken long-term, like those for hypertension, diabetes, or cancer. Antibiotics are generally taken for a short time, days to weeks usually, and don’t generate as much income.
What can be done bring more new antibiotics to market?
Last year a group of senators and representatives, including Michael Bennett (D-Colorado) introduced SB 2076, the PASTEUR Act. If passed, this will provide subscription contracts to developers of critical new antibiotics, enabling these companies to produce antibiotics to treat targeted critical infections. This will help treat antibiotic-resistant infections. There is also a plan for the Centers for Disease Control (CDC) to increase outreach to prescribers about antibiotic resistance and appropriate antibiotic prescribing.
How bad of a problem IS antibiotic resistance?
35,000 people die from antibiotic-resistant infections in the U.S. annually. There are nearly 3 million cases of resistant infections annually as well. During the early COVID pandemic, antibiotics were widely used for presumed secondary bacterial infections. Because antibiotic use greatly increased, antibiotic-resistant infections such as methicillin-resistant staphylococcus aureus (MRSA) also increased.
What causes antibiotic resistance?
The most common cause of resistance is inappropriate and over-use of antibiotics. This is the target of antibiotic stewardship programs at health facilities nationwide. As mentioned here (Treating c difficile: when the solution is part of the problem – Health, Hope, Healing (healthhopehealing.net)) antibiotics kill a wide range of both good and bad bacteria. Some strains of bacteria are able to mutate when exposed to certain antibiotics and these mutations allow them to evade an antibiotic that they were previously susceptible to. We are seeing this process play out in quick time with COVID variants.
Inappropriate use of antibiotics includes the following practices:
- Giving antibiotics for conditions that do not warrant them. For example, giving an antibiotic for a viral illness, like a cold.
- Giving an antibiotic for a condition that is over-diagnosed. For example, treating a sore throat with penicillin for strep, but not doing a strep test to confirm strep infection, as most sore throats are viral.
- Giving an antibiotic for a condition but using the wrong antibiotic. An example is using azithromycin to treat acute bacterial sinusitis. Azithromycin is not an appropriate antibiotic for that infection.
- Giving an antibiotic for a condition when a “watch and wait” strategy is appropriate but not used first. An example is giving children an antibiotic for an ear infection. Guidelines suggest waiting, as most cases of otitis media are viral and resolve on their own.
- Conditions where antibiotics are underused and timely need is not addressed, such as treating sexually transmitted infections.
Are there other prescribing problems that need to be addressed?
Yep! Many prescribers face barriers to appropriate antibiotic prescribing. There can be clinician knowledge gaps about best antibiotic prescribing practices and available clinical practice guidelines, crowded clinic schedules that don’t permit adequate time to address concerns, patients who demand antibiotics for inappropriate conditions, and clinician concerns about decreased patient satisfaction with clinical visits when antibiotics are not prescribed. These days, providers are paid in part upon patient satisfaction scores and on increased numbers of patients seen. Not a good recipe for quality care.
So, what can I do to get antibiotics appropriately?
Talk to your provider. If they are recommending an antibiotic, ask them why? What condition are they treating? Did they do a test to ensure their diagnosis? Are they following established guidelines for that condition? Are they giving you the right dose for the right duration of time? Speak up!
Antibiotics are necessary to treat bacterial infections. We will all need them from time to time. Adhering to established guidelines and appropriate prescribing practices can prevent the rise of new resistant infections and prevent needless adverse effects and secondary infections like c diff.
I will likely need a little break while I address a health concern. I’ll delve into the PASTEUR act next time – we need YOUR help! So please stay tuned! I’ll try and get it posted in the next week or two.
Also, starting this blog has been a big learning experience. I have a subscription button on my post page so you can receive an email with a link to my posts. I’m not sure if it is working just yet; please be patient while I figure it out.
Core Elements of Outpatient Antibiotic Stewardship | Antibiotic Use | CDC
What Is Antibiotic Stewardship—and How Does It Work? | The Pew Charitable Trusts (pewtrusts.org)
S.2076 – 117th Congress (2021-2022): PASTEUR Act of 2021 | Congress.gov | Library of Congress